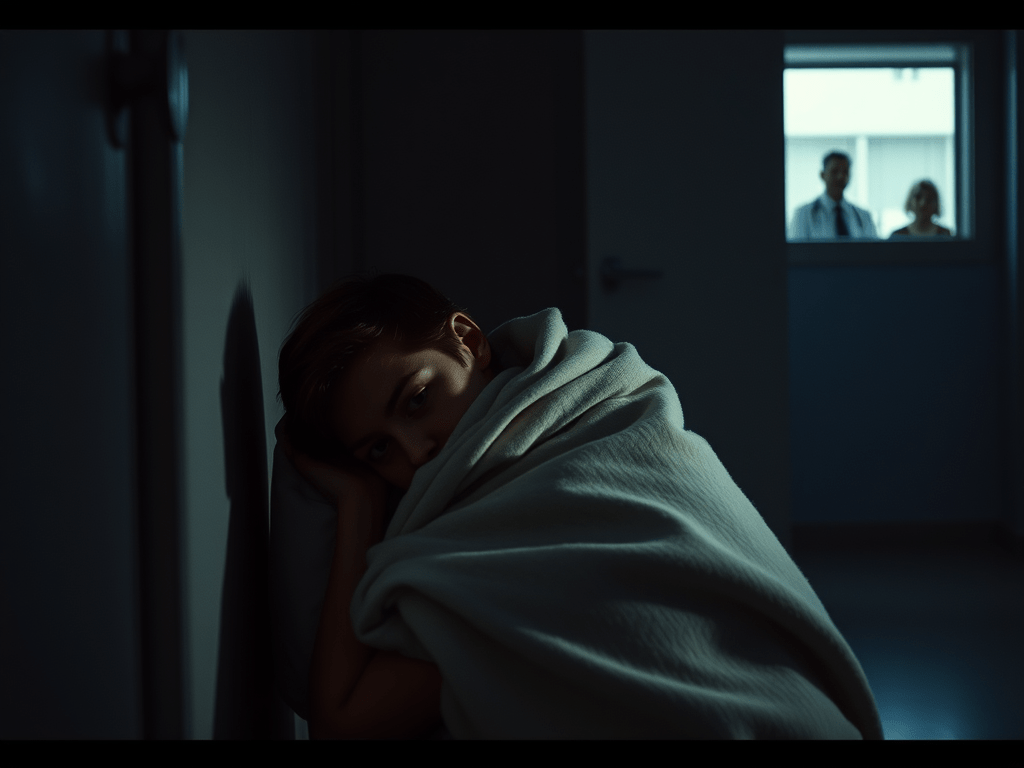
Sleepwalking again. Wandering into other rooms, trying to get out of the heavy, locked double doors to the psych unit. An MHT following me, attempting to talk to me. Not redirectable, I eventually wandered toward and attempted to get through the door to the interior part of the nurse station. Seclusion was right there and I was led into it, apparently wandering in willingly. I was locked in and walked in circles, sleeping deeply. I attempted to leave but the seclusion door was locked and I had no doorknob or latch to attempt to open it. Staff watched me through the window as I eventually curled up in the corner, leaning against the wall. Staff came in and did not attempt to wake me for fear of a violent reaction. They covered me with a blanket and I slept in seclusion, kept inside for “safety.” I woke to the door opening in the morning, confused, and alarmed.
“What happened??” I asked the MHT, frantically jumping up, the blanket in a pile at my feet.
“You were sleepwalking and some of your nighttime behaviors were unsafe, including trying to get out and going into other rooms as well as the nurse station. We guided you to seclusion for your safety. We were able to get you back to your bed but you got up again.”
He looked at me sympathetically as I was close to tears. It is frightening to wake up in a place that is not where you originally went to bed. “Can I come out?”
“Yes, it’s almost time for breakfast.”
I took a piss and splashed cold water on my face, trying to shake off the weird, disconcerting feeling. After breakfast was groups and my daily assessment.
“How do you feel about discharging in the next few days?”
“Yes, I want to.”
“I know you’ve been anxious to get home but do you really feel ready? Are you having thoughts of self harm?”
“I’m probably going to have some passive suicidal ideation forever. That’s my baseline. But no, I’ve been trying to plan some things. I write a lot.”
“I’ve noticed. Is that helpful for you?”
“Yeah it’s therapeutic. I can think a little straighter when I write.”
“Once you see the doctor today, we’ll formulate a plan for your discharge.”
That afternoon the doctor came. I was reading in my room, for the first time in a long time engaging in a leisure activity. I remember it was the third book in the Game of Thrones series. I was trying really hard to be more normal. I really hoped they would actually discharge me in a couple days.
“How are you feeling?”
“Better. I’m looking forward to going home.”
“I’m going to adjust your antipsychotic and increase the remeron for continued appetite stimulation. I saw you are up to 112 pounds now.”
“Yeah they weighed me this morning. I’ve been drinking the shakes, eating as much as I can. My stomach sometimes hurts. From the meds.”
“You’ve made an incredible improvement. I think after a couple days of med adjustments and lots of caloric intake, you’ll be ready for discharge. We’ll start safety planning tomorrow at your assessment.”
“Okay,” I nodded.
“You might want to see a sleep specialist. Talk to your doctor at the VA. You were difficult to redirect last night. You were placed in seclusion for safety.”
“Yeah it was weird to wake up in there.”
Safety planning can be hard. The next day I was asked what my triggers are, what are signs of decompensation, how do I know when to go to the hospital or at least call my doctor? I struggled with this back then because I had very little social support and was still trying to develop insight into my illness. I identified hearing voices, feeling suicidal, feeling like I can’t think straight or coherently (mania) quitting my meds, and paranoia. I agreed that these signs would get reported straight to my doctor when they happened to hopefully prevent decompensation from getting worse. I still struggle with this to this day. It’s hard to recognize when it’s happening and harder still to admit you’re weak, struggling, feeling suicidal or hearing voices.
My appetite was better. The remeron was working in that regard. I was trepidatious, worried about how to pick up the pieces when I got out, but the writing helped in that regard. I arranged a ride home with the only friend who knew I was in the hospital. She had been a second year grad student when I was a first year.
I was discharged a few days later, after a final assessment and thoroughly going over my safety plan. They gave me lots of brochures and papers about bipolar and PTSD, borderline, and tips on better management. They gave me a brochure about the 988 crisis line and strong encouragement to use it when I was struggling. They gave me papers on my medications, when to take them, and possible side effects to watch out for. I had a whole stack of papers when I finally walked out those doors and met my friend. I kept all my group papers as well.
My car was still at the VA from ages ago, when I was first detained there. My friend took me there but I had to go inside first and get my meds transferred to my provider. I set an appointment to see Heather in two days and went home, where my brother was waiting with my animals. The apartment was not such a mess as I kind of expected – I am a neat freak and my brother is nowhere near that. I decided to take a nap, catch my breath…and plan my next move.
Leave a comment